Related guidance:
Acne vulgaris: management NICE guideline (NG198 June 2021, updated May 2023)
Advise people with acne
- to use a non-alkaline (skin pH neutral or slightly acidic) synthetic detergent cleansing product twice daily on acne-prone skin.
- who use skin care products, sunscreens and make-up to avoid oil-based and comedogenic preparations and to remove make-up at the end of the day.
- persistent picking or scratching of acne lesions can increase the risk of scarring.
- there is not enough evidence to support specific diets for treating acne.
Urgently refer people with acne fulminans on the same day to the on-call hospital dermatology team, to be assessed within 24 hours.
- Refer people to a consultant dermatologist-led team if any of the following apply:
• there is diagnostic uncertainty about their acne
• they have acne conglobata
• they have nodulo-cystic acne. - Consider referring people to a consultant dermatologist-led team if they have:
• mild to moderate acne that has not responded to 2 completed courses of treatment
• moderate to severe acne which has not responded to previous treatment that contains an oral antibiotic
• acne with scarring
• acne with persistent pigmentary changes. - Consider referring people to a consultant dermatologist-led team if their acne of any severity, or acne-related scarring, is causing or contributing to persistent psychological distress or a mental health disorder.
- Consider referral to mental health services if a person with acne experiences significant psychological distress or a mental health disorder, including those with a current or past history of:
• suicidal ideation or self-harm
• a severe depressive or anxiety disorder
• body dysmorphic disorder. - Consider condition-specific management or referral to a specialist (for example a reproductive endocrinologist), if a medical disorder or medication (including self-administered anabolic steroids) is likely to be contributing to a person’s acne.
Acne vulgaris patient information leaflet (British Association of Dermatologists July 2020)
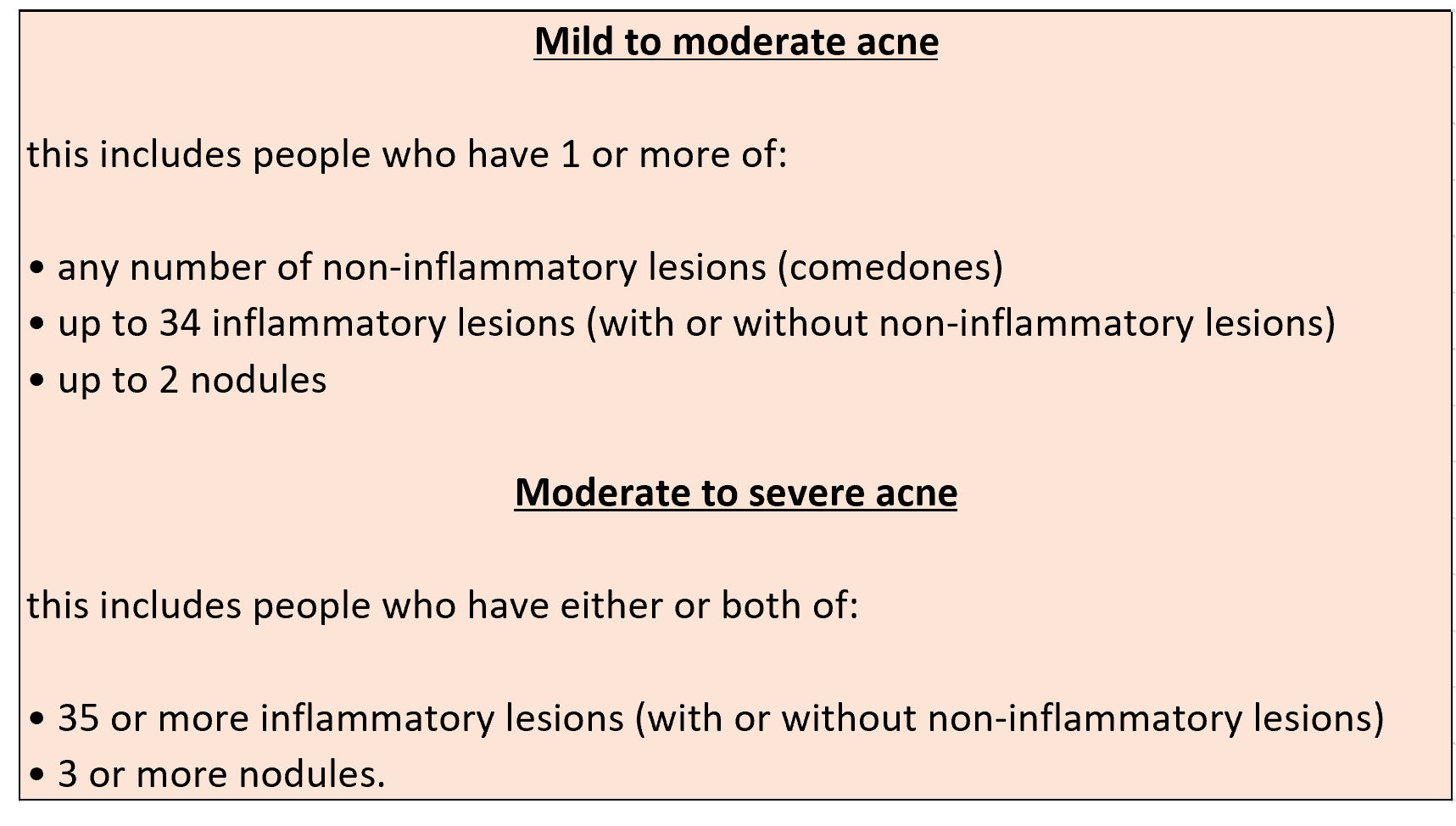
- Acne severity varies along a continuum.
Treatment
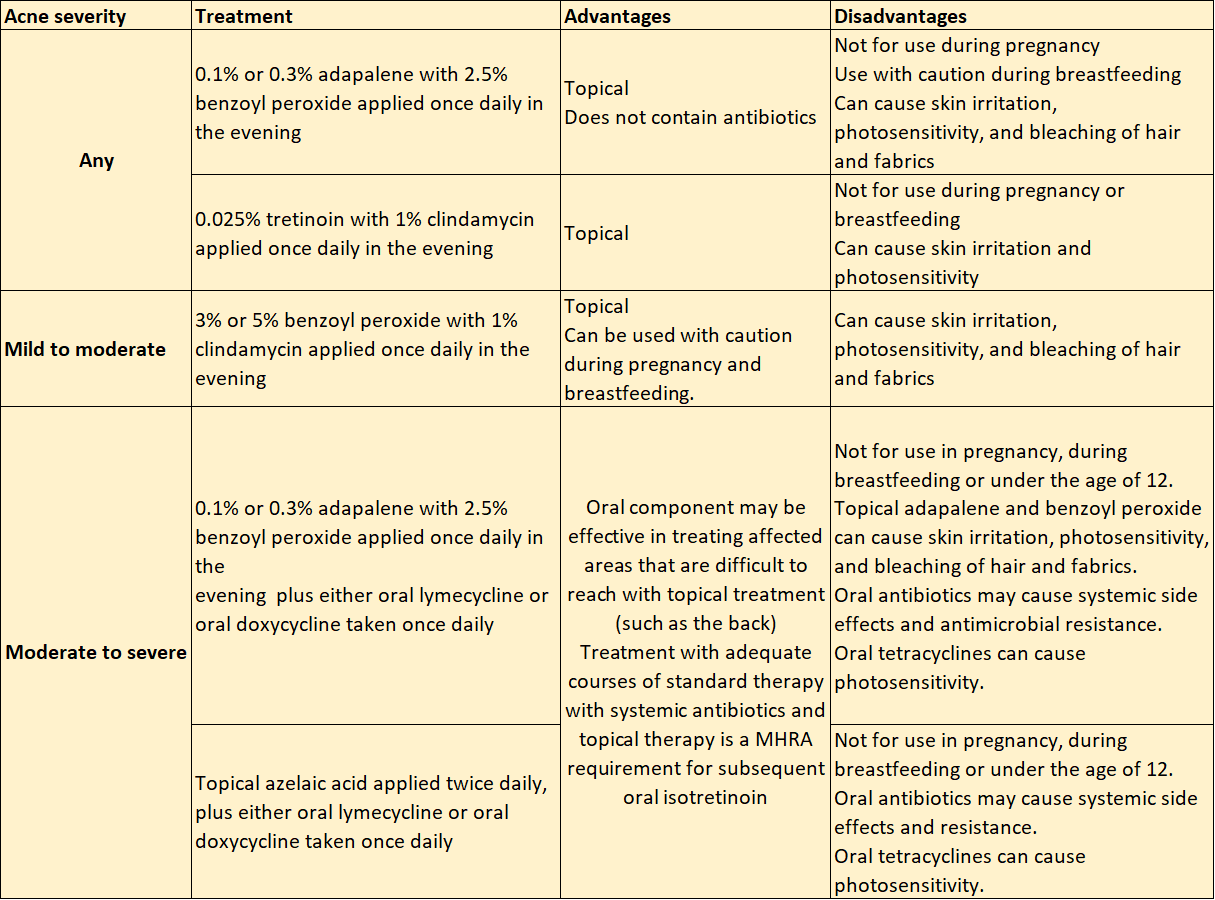
- Offer people with acne a 12-week course of 1 of the following first-line treatment options, taking account of the severity of their acne and the person’s preferences, and after a discussion of the advantages and disadvantages of each option.
- Consider topical benzoyl peroxide monotherapy as an alternative treatment to the options if:
• these treatments are contraindicated, or
• the person wishes to avoid using a topical retinoid, or an antibiotic (topical or oral). - For people with moderate to severe acne who cannot tolerate or have contraindications to oral lymecycline or oral doxycycline, consider replacing these medicines in the combination treatments with erythromycin.
- Take into account that acne of any severity can cause psychological distress and mental health disorders.
- Discuss the importance of completing the course of treatment, because positive effects can take 6 to 8 weeks to become noticeable.
- Take into account that the risk of scarring increases with the severity and duration of acne.
- To reduce the risk of skin irritation associated with topical treatments, such as benzoyl peroxide or retinoids, start with alternate-day or short-contact application (for example washing off after an hour). If tolerated, progress to using a standard application.
- When discussing treatment choices with a person with childbearing potential, cover:
• that topical retinoids and oral tetracyclines are contraindicated during pregnancy and when planning a pregnancy and
• that they will need to use effective contraception, or choose an alternative treatment to these options. - If a person receiving treatment for acne wishes to use hormonal contraception, consider using the combined oral contraceptive pill in preference to the progestogen-only pill if oral isotretinoin treatment is likely to be used.
NHS Somerset classify oral isotretinoin as a red drug (specialist prescribing only) as per Traffic light guidance.
- If clinical judgement indicates a person may need treatment with oral isotretinoin for their acne in future:
• be aware that oral isotretinoin should not be used unless adequate courses of standard therapy with systemic antibiotics and topical therapy have been tried.
• take this into account when choosing any initial treatment option. - Explain that isotretinoin can cause serious harm to a developing baby if taken during pregnancy
• inform them that they will need to follow the MHRA pregnancy prevention programme. - If a person is taking oral isotretinoin for acne:
• review their psychological wellbeing during treatment, and monitor them regularly for symptoms or signs of developing or worsening mental health problems or sexual dysfunction
• tell them to seek medical advice if they feel their mental health or sexual function is affected or is worsening, and to stop their treatment and seek urgent medical advice if these problems are severe. - Follow the MHRA guidance on important risks and precautions for isotretinoin.
This includes:
- prescribing only by a consultant dermatologist-led team
- assessing and monitoring mental health
- assessing and monitoring sexual function. - Do not use the following to treat acne:
• monotherapy with a topical antibiotic
• monotherapy with an oral antibiotic
• a combination of a topical antibiotic and an oral antibiotic. - Review first-line treatment at 12 weeks and:
• assess whether the person’s acne has improved, and whether they have any side effects
• in people whose treatment includes an oral antibiotic, if their acne has completely cleared consider stopping the antibiotic but continuing the topical treatment
• in people whose treatment includes an oral antibiotic, if their acne has improved but not completely cleared, consider continuing the oral antibiotic, alongside the topical treatment, for up to 12 more weeks. - Only continue a treatment option that includes an antibiotic (topical or oral) for more than 6 months in exceptional circumstances. Review at 3-monthly intervals, and stop the antibiotic as soon as possible.
- Be aware that the use of antibiotic treatments is associated with a risk of antimicrobial resistance.
- If a person’s acne has cleared, consider maintenance options.
- If acne fails to respond adequately to a 12-week course of a first-line treatment option and at review the severity is:
• mild to moderate: offer another option of treatment choices.
• moderate to severe, and the treatment did not include an oral antibiotic: offer another option which includes an oral antibiotic of treatment choices.
• moderate to severe, and the treatment included an oral antibiotic: consider referral to a consultant dermatologist-led team. - If mild to moderate acne fails to respond adequately to 2 different 12-week courses of treatment options, consider referral to a consultant dermatologist-led team.
- Photodynamic therapy can be considered for people aged 18 and over with moderate to severe acne if other treatments are ineffective, not tolerated or contraindicated.
- For people with polycystic ovary syndrome and acne:
• treat their acne using a first-line treatment option
• if the chosen first-line treatment is not effective, consider adding ethinylestradiol with cyproterone acetate (co-cyprindiol) or an alternative combined oral contraceptive pill to their treatment.
• for those using co-cyprindiol, review at 6 months and discuss continuation or alternative treatment options. - Consider referring people with acne and polycystic ovary syndrome with additional features of hyperandrogenism to an appropriate specialist (for example, a reproductive endocrinologist).
Relapse
- If acne responds adequately to a course of an appropriate first-line treatment but then relapses, consider either:
• another 12-week course of the same treatment, or
• an alternative 12-week treatment. - If acne relapses after an adequate response to oral isotretinoin and is currently mild to moderate, offer an appropriate treatment option.
- If acne relapses after an adequate response to oral isotretinoin and is currently moderate to severe, offer either:
• a 12-week course of an appropriate treatment option, or
• re-referral, if the person is no longer under the care of the consultant dermatologist-led team. - If acne relapses after a second course of oral isotretinoin and is currently moderate to severe, further care should be decided by the consultant dermatologist-led team. If the person is no longer under the care of the consultant dermatologist-led team, offer re-referral.
Maintenance
- Encourage continued appropriate skin care.
- Explain to the person with acne that, after completion of treatment, maintenance treatment is not always necessary.
- Consider maintenance treatment in people with a history of frequent relapse after treatment.
- Consider a fixed combination of topical adapalene and topical benzoyl peroxide as maintenance treatment for acne. If this is not tolerated, or if 1 component of the combination is contraindicated, consider topical monotherapy with adapalene, azelaic acid, or benzoyl peroxide.
- Review maintenance treatments for acne after 12 weeks to decide if they should continue.
Management of acne-related scarring
- If a person has acne-related scarring, discuss their concerns and provide information in a way that suits their needs. Topics to cover include:
• possible reasons for their scars
• treatment of ongoing acne to help prevent further scarring
• possible treatment options for acne-related scarring
• the way their acne scars may change over time
• psychological distress. - If a person’s acne-related scarring is severe and persists a year after their acne has cleared:
• refer the person to a consultant dermatologist-led team with expertise in scarring management
• in a consultant dermatologist-led team setting, consider CO2 laser treatment (alone or after a session of punch elevation) or glycolic acid peel.
NHS Somerset Medicines used in pregnancy
| Therapeutic Area | Formulary Choices | Cost for 28 (unless otherwise stated) | Rationale for decision / comments |
|---|---|---|---|
| Retinoid and related drugs | Adapalene and benzoyl peroxide as Epiduo® | 0.1 and 2.5% gel: £19.53 (45g) | For Acne. Apply once daily in the evening. Not for use during pregnancy. Use with caution during breastfeeding. Can cause skin irritation, photosensitivity, and bleaching of hair and fabrics. |
| 0.3 and 2.5% gel: £19.53 (45g) | |||
| Tretinoin and clindamycin as Treclin® | 0.025 and 1% gel: £11.94 (30g) | For Acne. Apply once daily in the evening for 12 weeks. Not for use during pregnancy or breastfeeding. Can cause skin irritation and photosensitivity. |
|
| Trifarotene | 50mcg/g cream: £27.75 (75g) | For treatment of Acne Vulgaris of the face and/or the trunk in patients from 12 years of age and older, when many comedones, papules and pustules are present. Child 12–17 years and adults: apply once daily, to be applied thinly in the evening. Avoid contact with eyes, nostrils, mouth and mucous membranes, eczematous, broken or sunburned skin; avoid exposure to UV light (including sunlight, sunlamps) The MHRA advises females of childbearing potential should use effective contraception. |
|
| Antiseptics and disinfectants, peroxides | Benzoyl peroxide as | 5% gel: £5.44 (30g), £10.68 (60g) 5% wash gel: £8.81 (100g) | For Acne. Apply once or twice daily. Can be used with caution during pregnancy and breastfeeding. Ensure topical treatments don't come into contact with child's skin if breastfeeding. Can cause skin irritation, photosensitivity, and bleaching of hair and fabrics. |
| Benzoyl peroxide and clindamycin as Duac®Once Daily | 3 and 1% gel: £13.14 (30g), £26.28 (60g) | For Acne. Apply once daily in the evening for 12 weeks. Can be used with caution during pregnancy and breastfeeding. Ensure topical treatments don't come into contact with child's skin if breastfeeding. Can cause skin irritation, photosensitivity, and bleaching of hair and fabrics. |
|
| Erythromycin and zinc acetate as Zineryt® | 40mg/ml and 12mg/ml lotion: £9.25 (30ml), £20.02 (90ml) | For Acne. Apply twice daily for 10-12 weeks. For people who cannot tolerate or have contraindications to other options. Can be used with caution during pregnancy and breastfeeding. Ensure topical treatments don't come into contact with child's skin if breastfeeding. |
|
| Antibacterials, Tetracyclines and related drugs | Lymecycline | 408mg capsule: £4.79 (28), £9.58 (56) | For Acne. Take one capsule once daily. Not for use in pregnancy, during breastfeeding or under the age of 12. Oral antibiotics may cause systemic side effects and antimicrobial resistance. Oral tetracyclines can cause photosensitivity. |
| Doxycycline | 100mg capsule: £1.05 (8) | ||
| Antibacterials, Macrolides | Erythromycin | 250mg gastro-resistant tablet: £1.60 (28) | For Acne. Take one to two tablet twice daily. For people who cannot tolerate or have contraindications to oral lymecycline or oral doxycycline. |
| Anticomedonals | Azelaic acid as Finacea® | 15% gel: £7.48 (30g) | For acne and rosacea. Apply twice daily. |
| Azelaic acid as Skinoren® | 20% cream: £4.49 (30g) | ||
| Anti-androgens | Co-cyprindiol (Cyproterone acetate/ethinylestradiol) as Dianette® | 2mg/35mcg tablet: £7.71 (63) | For Acne. The risk of VTE with Co-Cyprindiol is higher than with conventional low-dose COCPs and it is recommended that: • it should only be used if the chosen first-line treatment is not effective • it should only be used in licensed indication • it should not be used solely for contraception • for those using co-cyprindiol, review at 6 months and discuss continuation or alternative treatment options. |
| NHS Somerset classify oral isotretinoin as a red drug (specialist prescribing only) as per Traffic light guidance. |
|||
| Teratogenic risk | New prescriber checklists, patient reminder cards, and pharmacy checklists are available to support the Pregnancy Prevention Programme in women taking acitretin, alitretinoin, and isotretinoin. Advice about the risk of neuropsychiatric reactions has been made consistent for all oral retinoid medicines. See MHRA Drug Safety Update (June 2019) for Oral retinoid medicines: revised and simplified pregnancy prevention educational materials for healthcare professionals and women. | ||
| Isotretinoin should only be used for severe forms of acne resistant to adequate courses of standard therapy with systemic antibacterials and topical therapy. Prescription of isotretinoin should be supervised by specialist dermatologists with a full understanding of the potential risks and monitoring requirements. See MHRA Drug Safety Update (August 2020) for Isotretinoin: reminder of important risks and precautions. | |||
| The Isotretinoin Expert Working Group of the Commission on Human Medicines has made recommendations to strengthen the safety of isotretinoin treatment. Recommendations include new warnings, the need for consistent monitoring requirements for psychiatric side effects, the introduction of new monitoring requirements for sexual side effects, and additional oversight of the initiation of treatment for patients younger than 18 years. See MHRA (April 2023) for Isotretinoin (Roaccutane▼): new safety measures to be introduced in the coming months, including additional oversight on initiation of treatment for patients under 18 years. | |||
| Antibacterials, Nitroimidazole derivatives | Metronidazole as Rozex® | 0.75% cream: £6.60 (30g) £9.88 (40g) 0.75% gel: £6.60 (30g) £9.88 (40g) | For Rosacea. Apply twice daily. |
| Acea® | 0.75% gel: £9.95 (40g) | For Rosacea. Apply twice daily. | |
| Anthelmintics | Ivermectin as Soolantra® | 10mg/g cream: £27.43 (45g) | For Rosacea if other options tried. Apply daily. |
| Sympathomimetics, Alpha2-adrenoceptor agonists | Brimonidine as Mirvaso® | 3mg/g gel: £33.69 (30g) | |
| Some patients may have exacerbation or rebound symptoms of rosacea. It is important to initiate treatment with a small amount of gel and increase the dose gradually, based on tolerability and treatment response. See MHRA Drug Safety Update (November 2016) for for Brimonidine gel: risk of exacerbation of rosacea. | |||
| Systemic cardiovascular effects including bradycardia, hypotension, and dizziness have been reported after application. It is important to avoid application to irritated or damaged skin, including after laser therapy. See MHRA Drug Safety Update (June 2017) for Brimonidine gel: risk of systemic cardiovascular effects; not to be applied to damaged skin. | |||